Designing and
Implementing a Telemedicine System.
Type of
article: Original
Abstract
Background:
A modern Teleconsultation System (TCS)
improves patients' monitoring and favors remote assistance in terms of
facilitating the daily life to the patients. This work investigates how to
design and implement a modern remote consultation system.
Methods: To achieve this work, we identify the actors who interact with the system
to be developed and the use cases relating to each actor. A class model is
designed to derive the relational model and the corresponding database. During
implementation, we have used PHP language and MySQL database system.
Results: A
tele-consultation framework is implemented. The users (patients and doctors)
must register then authenticate in order to use the system. The latter allows
them audio and video conversation between them.
Conclusion: We have
given in this study how to design and implement a telemedicine system which
will improve health care, ensure continuity and quality of homecare while
inhibiting intercurrences or complications, which will limit hospital
admissions and limit medical travel.
Keywords: Telemedicine,
Tele-consultation, Healthcare, Medical remote system.
Corresponding author: r:AbderrazakSebaa,Department
of Computer Science, University of Bejaia, Algeria Email:
balzak.sebaa@gmail.com
Received: 29
June, 2018, Accepted: 28 December, 2018, English editing: 03 January,
2019,Published: 09 January, 2019.
©2017-2018
KNOWLEDGE KINGDOM PUBLISHING.
1. Introduction
1.1. Background and the problem specification
Developing countries are severely lacking
healthcare infrastructure and staff. Indeed, these countries suffer from
understaffed hospitals and community services especially the specialists. This
situation spawned health inequalities between different regions and population [1].
When talking about the qualifications and
distribution of health personnel, the WHO (World Health Organization) considers
it unlikely that countries with fewer than 23 health professionals (counting
only the doctors, the nurses, and midwives) per 10,000 population obtain
appropriate coverage rates for essential interventions in primary healthcare
that are prioritized by the development intentions for the millennium [2].
Thus, considering the vastness of the Algerian
territory, the number of the health personnel and based on the recommendations
of WHO, the medical coverage is not fully ensured especially in the remote
zones of the country. Telemedicine can solve partially this problem.
Teleconsultation (TC), in particular, become a necessity or even an obligation
for greater equity in the availability of healthcare specialists throughout the
country. By telemedicine it is meant a form of remote therapeutic practice
linking a patient and one or more healthcare specialists via Information and
Communication Technologies (ICTs). Different categories of telemedicine,
including: tele expertise, telemonitoring, tele assistance, and finally, teleconsultation.
1.2. Objectives
This work focuses
on achieving a telemedicine system. The proposed Teleconsultation System (TCS)
will connect patients, caretakers and health staff. It will allow consultation
and diagnosis of patients remotely fulfilling the following objectives:
- To ensure the quality
as well as the continuity of homecare;
- To prevent
complications and thus limit hospitalizations;
- Limit travel and
facilitate access to care in remote areas;
- To shorten waiting
times; and
- To increase the medical
coverage of users of the healthcare system and to follow-up patients with
chronic illnesses or incapacities [3].
2. Materials and Methods
Referring to the 2TUP
approach covering all steps involving the analysis phase to the system design
which represents two essential stages of our conception process. The initial
functional structure comprises class models and use cases for the different
actors: the physician, governmental agencies, the administrator, the caretaker
and the patient). The proposed architecture entails a 3-tier architecture style
that relates the client applications and the database server. The next
subsections describe materials and methods.
2.1 Materials
In order to properly design
our tele-consultation system, we design the use cases diagram and the class
model of our framework. Noting that the last one is used to obtain the
relational model (required in our application) using passing rules to be used
in our application. The implementation of the system was made by PHP language,
the querying and databases were implemented with MySQL which is compatible with
PHP.
2.2 Methods
Realizing a
telemedicine system is a complex task which consists of several phases:
designing phase which includes requirements identification, actors’
identification, and UML modeling. Then, the implementation phase which consists
of databases, interfaces, and communication tools implementation.
The project requirements are
twofold. Functional requirements for the TCS must allow a trustworthy and
confidential communication among all the actors. Non-functional requirements
which mean to ensure a secure communication, processing speed, and performance.
2.2.1 Uses cases
This use case diagram involves the information system general modeling
where there is the root actor "user" that has as only case of use
"registration" and it is inherited by three other actors
"administrator", "doctor" and "patient". The
administrator has a single use case "User Management" to manage
physicians and patients and that directly includes an authentication.
The doctor has four use cases: "Patient Management" to manage
patients, "Prescription Management" for giving and writing of medical
prescriptions, and two other use cases shared with the actor
"Patient." These shared cases are, respectively, "Appointment
Management" for making appointments, and "Conversation
Management" to manage conversations among patients, caretakers and
doctors. The latter actor "Patient" has two specific use cases,
namely, "Medical samples" and "Prescription consulting". In
all these use cases, an actor must receive authentication first.
The
next step is the data model elaboration, which must specify the system to
accept expansions to accommodate present and forthcoming requirements.

Figure 1:
Uses cases of the TCS.
2.2.2 Data modeling
The simplest UML diagram is
the class diagram. The static system view is shown through this diagram, comprising
classes, their interrelations including generalization, specialization,
relationship, aggregation, composition, operations and attributes [4]. Thus,
this diagram contains the attributes to implement all the classes exposed in
Figure 2 are necessary for the application modeling. Starting with the class
"user," which is inherited by the pair of classes: "doctor"
and "patient". Then, the class "Appointment" is requested
by the patient and validated by the doctor. Right after two association classes
appear: "Message," which classifies it for the conversations, and
"consultation," which is related to the classes "Therapy"
" and "Report" by the relations <father rt"
<father-son>. Coming back to the "patient" that has a
<father father-son> relationship with the class "additional
information" which gives the inheritance to the last three classes
"Glycemia", "Weight" and "blood pressure".
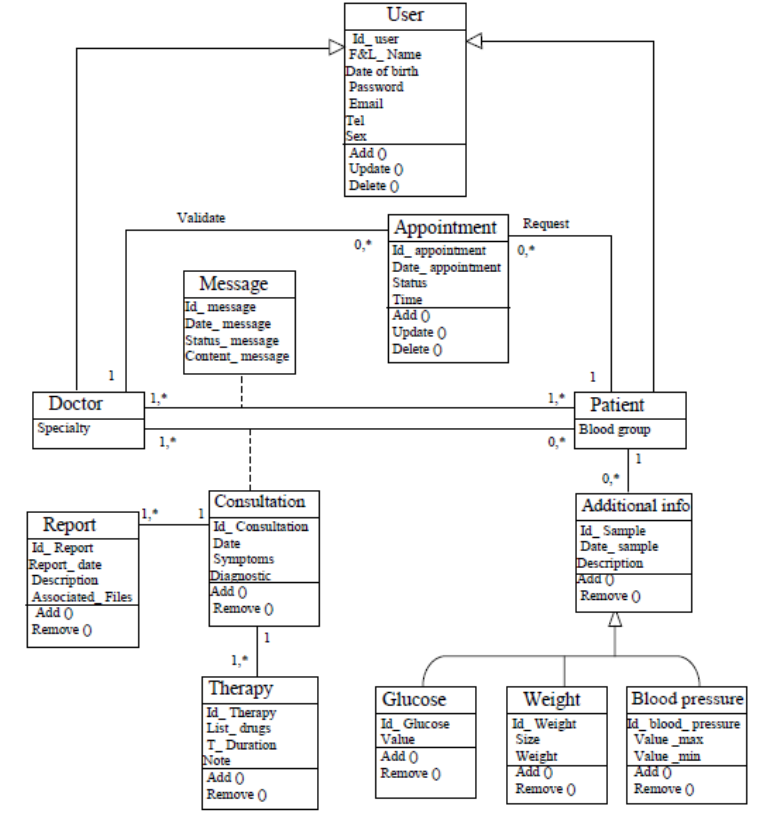
Figure 2: Class diagram of the tele-consultation
system.
2.2.3 Tele-consultation system implementation
Some software packages for the implementation
of Web-based applications have been investigated relying on several parameters,
e.g., administration tools, deployment and maintenance strategies, data
confidentiality, information integrity,
concurrency regulation, data backup and restore existing procedures and
software learning curves. As far as software goes the teleconsultation
application system uses a MySQL database.
2.3 Ethical aspects
Protection and confidentiality about patients’
personal information: Patients’ particular data like first name, last name,
native land, and date of birth demand system protection. This can be
accomplished by an identifier and the patient’s age. Only those directly
involved with the TCS development, healthcare provision and the medical
administration have access to medical information items.
3. Results
The subsequent aspects of the designed TCS
will be investigated:
(a) Inscription;
(b) Authentication;
(c) Doctor’s appointments list;
(d) Patient interface;
(e) Doctors and Patients management; and
(f) Creation of the medical staff accounts
relation.

Figure 3: Main TCS interfaces.
The recommended TCS allows to access a
physician remotely. The user (patient) remotely begins with the homepage by
first authenticating his credentials (Figure 3.a). If an account associated to
his name is not found, then he must register (Figure 3.b). If a doctor is
available (Figure 3.c), the patient will access the appointments' list for the
sake of perusal and to contact the patient through messages and a video call.
When the consultation ends, he can prescribe tact medications through an
electronic prescription. If the operator tries to enter a patient account
(Figure 3.d), then he can choose a doctor to treat and make an available appointment
and see the previous messages with his chosen doctor as he can contact ointment
him. The administrator of the application can make modifications, deletions of
doctors and patients (Figure 3.e) and also create medical staff accounts
(Figure 3.f). The subsequent diagram (Figure 4) illustrates the interaction
between a physician and a patient via tele-consultation. So, the TCS will give
assistance and medical diagnostic to patients remotely.
Figure 4. Remote interaction between
a physician and patient.
4. Discussion
Numerous studies [4, 5, 6]
have recommended telemedicine to improve healthcare quality of patients.
Several telemedicine applications examples have been developed by Kvedar et al.
[7], and these many examples show the potential of telemedicine system for
healthcare access improving quality, and efficiency in healthcare and
telemedicine.
However, little efforts have
addressed telemedicine systems in Algeria. To begin with, the slow adoption of
telecommunication technology in Algeria has introduced some challenges.
Secondly, is that the direction and effort of the country are directed he
towards the ensuring of enough number of doctors. Only the Algerian Advanced
Technology Development Center he (CDTA) has developed the only Algerian telemedicine
platform for some Algerian hospitals [8]. Nevertheless, many Algerian other
hotels, health centers and private medical professionals still do not have this
solution or are not apt to use the telemedicine systems. The proposed TCS
solution simplifies communications between patients and doctors, and it allows
managing diverse patient' information. However, it is better to enrich it with
other features. Furthermore, privacy policies regarding patients' data due to
the delicate nature of medical/healthcare information are paramount for
telemedicine.
Future developments will
analyze solutions from other places and how they can be translated to Algeria
[9, 10, 11, 12]. Moreover, provisions for intelligent information retrieval and
database handling must be thought [13, 14].
5. Conclusions
Telemedicine is a promising alternative
solution to provide healthcare to distant to reach or underdeveloped areas.
Several novel medical technologies and research projects are currently being
considered for the sake of easy deployment and implementation. This manuscript
has examined the design of a telemedicine system for medical tele-consultation
relying on a Web application. This medical remote structure reduces distances
and facilitates collaboration between healthcare organizations, healthcare
professionals, patients and caretakers by using communication technology and
data transmission techniques. Our solution provides an interesting resolution
for issues of many levels, namely economical, medical, social, and technical.
Nevertheless, enriching this solution with other features will give superior
results. Furthermore, since medical data is extremely sensitive and involve
privacy, it is important to enforce and deploy robust privacy policies of
patients' data.
Acknowledgments The authors sincerely
thank the anonymous reviewers for their comments on the final manuscript and
their valuable feedback.
6. Conflict of interest statement
Authors
declare no conflicts of interest.
7. Authors biography
Hachemi Atroune is a Master Student in the Department of Computer science of Exact
Sciences Faculty at Mira Abderahmane University, Bejaia, Algeria.
Abderrazak Sebaa is currently Associate Professor with the Department of Computer science
and searcher at LIMED laboratory, at Mira Abderahmane University, Bejaia,
Algeria. He received his Ph.D. degree in computer science from the same
university.
Koceila Chefai is a Master Student in the Department of Computer science of Exact
Sciences Faculty at Mira Abderahmane University, Bejaia, Algeria.
Lydia Abbas is a Master Student in the Department of Computer science of Exact
Sciences Faculty at Mira Abderahmane University, Bejaia, Algeria.
Nesrine Hammouche is a Master Student in the Department of Computer science of Exact
Sciences Faculty at Mira Abderahmane University, Bejaia, Algeria.
Yamina Khiati is a Master Student in the Department of Computer science of Exact
Sciences Faculty at Mira Abderahmane University, Bejaia, Algeria.
8. References
1) Sebaa, A., Nouicer, A.,
Tari, A., Tarik, R., & Abdellah, O. (2017). Decision support system for
health careresources
allocation.Electronic physician, 9(6), 4661.
https://doi.org/10.19082/4661
PMid:28848645 PMCid:PMC5557150
2) World Health
Organization. World Health Statistics 2016. In World Health Statistics. Visited
2016
3) Solutions medicales, La télémédecine,
définition et mise en oeuvre.
http://solutionsmedicales.fr/.
Visited 2012.
4) Szlenk, M. (2006, May).
Formal semantics and reasoning about uml class diagram. In
Dependability ofComputer
Systems, 2006. DepCos-RELCOMEX'06. International Conference
on (pp. 51-59). IEEE.
https://doi.org/10.1109/DEPCOS-RELCOMEX.2006.27
5) Paré, G., Jaana, M.,
& Sicotte, C. (2007). Systematic review of home telemonitoring for
chronic diseases:
theevidence base.Journal of the American Medical Informatics Association,
14(3), 269-277
https://doi.org/10.1197/jamia.M2270 PMid:17329725 PMCid:PMC2244878
6) Roine, R., Ohinmaa, A.,
& Hailey, D. (2001). Assessing telemedicine: a systematic review of
theliterature. Canadian
Medical Association Journal, 165(6), 765-771.
PMid:11584564
PMCid:PMC81454
7) Kvedar, J., Coye, M. J.,
& Everett, W. (2014). Connected health: a review of technologies and
strategies toimprove
patient care with telemedicine and telehealth. Health Affairs, 33(2), 194-199.
Medical Technologies
Journal, Volume: 2, Issue: 4, January-March 2018, Pages:277-284.
Doi
:https://doi.org/10.26415/2572-004X-vol2iss1p277-284
284
https://doi.org/10.1377/hlthaff.2013.0992
PMid:24493760
8) Oudjoudi, I. (2017). Plateforme
télémédecine au service des populations enclavées en Algérie.
Deuxièmes Journées Internationales du centre
anti-cancer Annaba, 07 et 08 Janvier 2017
9) Vermesan O, Friess P
(eds) (2015) Building the hyperconnected society: IoT research and
innovation value chains,
ecosystems and markets. River Publishers, Denmark
https://doi.org/10.13052/rp-9788793237988
10) Thuemmler C, Mival O,
Benyon D et al (2013) Norms and standards in modular medical
architectures. In: Proc. of
the IEEE HealthCom 2013.
https://doi.org/10.1109/HealthCom.2013.6720705
11) Seger, W. "The
Rediscovery of the Social Side of Medicine: Philosophy and Value of the
International
Classification of Functioning, Disability and Health (ICF)". Medical
Technologies
Journal, Vol. 1, no. 1,
Mar. 2017, pp. 3-3, doi:https://doi.org/10.26415/2572-004X-vol1iss1p3-3.
12) Belgherbi, A., I.
Hadjidj, and A. Bessaid. "Computer-Aided Detection of Simultaneous
Abdominal Organ from CT
Images Based on Iterative Watershed Transform". Medical
Technologies Journal, Vol.
1, no. 1, Mar. 2017, pp. 8-8,
doi:https://doi.org/10.26415/2572-004Xvol1iss1p8-8.
https://doi.org/10.26415/2572-004X-vol1iss1p8-8
13) Jesus, M.A., &
Estrela, V.V. (2017). An Introduction to Data Mining Applied to HealthOriented
Databases.Orient. J. Comp. Sci. and Technol (OJCST), 9(3). DOI:
10.13005/ojcst/09.03.03
https://doi.org/10.13005/ojcst/09.03.03
14) Herrmann, A. E. &
Estrela, V. V. (2016). Content-based image retrieval (CBIR) in remote
clinical diagnosis and
healthcare. In M. Cruz-Cunha, I. Miranda, R. Martinho, & R. Rijo (Eds.),
Encyclopedia of E-Health
and Telemedicine (pp. 495-520). Hershey, PA: IGI Global.
doi:10.4018/978-1-4666-9978-6.ch039 https://doi.org/10.4018/978-1-4666-9978-6.ch039